-
- Global AMC MENU
- NEWS
- HEALTH
- PEOPLE
- Introduction
Anticoagulants, lower incidence of leaflet thrombosis
World's first to prove no correlation between the occurrence of leaflet thrombosis and cerebral lesions or neurological/neurocognitive function
"Resolving concerns about cerebral thromboembolism after TAVR and determining antithrombotic agents according to patient conditions"
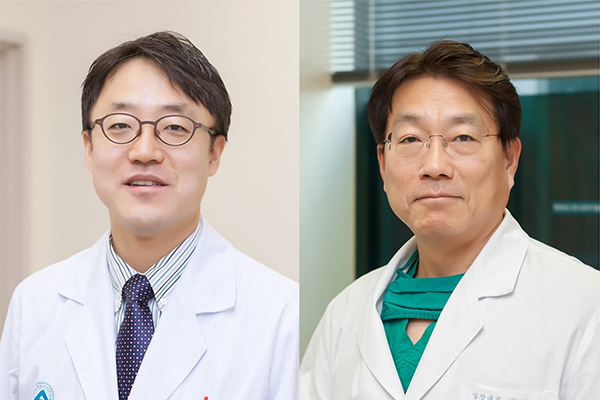
▲(from the left) Professor Duk-Woo Park and Professor Seung-Jung Park
Transcatheter Aortic Valve Replacement (TAVR), which has become the standard treatment for aortic stenosis, is performed worldwide, including Korea, gaining high satisfaction among high-risk patients such as the elderly or critically-ill.
It is known that thrombosis occurs around the replaced artificial heart valve after TAVR. Concerns arose that if the valve's bloodstream moves to the brain, it may cause cerebral thromboembolism or neurological/neurocognitive dysfunction.
To prevent this, appropriate antithrombotic agents should be taken after TAVR. Even though studies have found that anticoagulant agents are more effective than dual antiplatelet therapy (DAPT), a clear correlation has not yet been revealed.
AMC team led by Professor Duk-Woo Park and Professor Seung-Jung Park of the Division of Cardiology conducted an international multicenter clinical study of 229 people who underwent successful TAVR in Korea, Hong Kong, and Taiwan through open-label randomized trial comparing anticoagulant edoxaban with dual antiplatelet therapy (DAPT; aspirin plus clopidogrel). As a result, there was a lower incidence of leaflet thrombosis in the edoxaban group (9.8%) than in the DAPT group (18.4%), but there was no difference in the incidence of cerebral thromboembolism and neurological or neurocognitive function between two groups.
The findings were selected as the '2022 Late-Breaking Clinical Trial' of the American College of Cardiology (ACC), a medical association in cardiology with the highest authority. Professor Duk-Woo Park, the principal investigator, presented the results at the ACC 2022 Scientific Session held in Washington DC, US from April 2nd to 4th. Simultaneously, the results were published in the latest online issue of ‘Circulation’ (Impact Factor=29.69), a prestigious journal in the field of cardiovascular diseases.
After TAVR, antithrombotic agents such as anticoagulants and antiplatelet agents are taken to prevent blood clots in the valve. Anticoagulants are more effective in preventing blood clots than antiplatelet agents, but are mainly used in patients with high risk of thrombosis such as the elderly or with arrhythmia because they have a higher risk of bleeding.
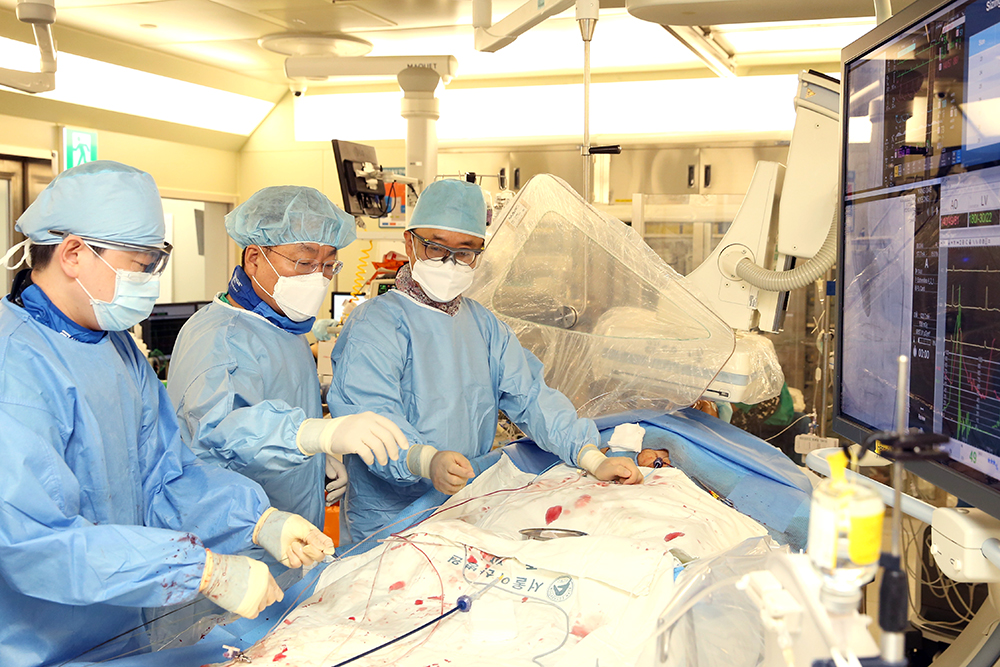
▲Professor Duk-Woo Park and Professor Seung-Jung Park (from the right) performing TAVR
Professor Duk-Woo Park and Professor Seung-Jung Park of the Division of Cardiology conducted a randomized clinical trial comparing the effects of anticoagulants and dual antiplatelet therapy (DAPT) to overcome the limitations of empirically based on expert consensus and resolve uncertainties about the causal relationship of subclinical leaflet thrombosis and cerebral thromboembolism.
The research team randomly assigned anticoagulants (edoxaban, 111 patients) and DAPT (aspirin plus clopidogrel, 118 patients) to 229 patients who underwent TAVR in five medical institutions of Korea, Hong Kong, and Taiwan and monitored them for six months. The mean age of patients was 80 years old and 58% of the patients were women.
As a result of performing cardiac CT scans after 6 months, the incidence of leaflet thrombosis in the anticoagulant group was 9.8% and was 18.4% in DAPT group. After TAVR, anticoagulant therapy was found to be more effective in preventing leaflet thrombosis than DAPT.
On the other hand, MRI and neurocognitive function tests were performed twice, immediately within a week and six months after TAVR. There was no difference in the incidence of cerebral thromboembolism and neurological or neurocognitive function between the anticoagulant group and the DAPT group. It also proved that there was no clear correlation between the occurrence of leaflet thrombosis and cerebral lesions or neurological/neurocognitive function after TAVR.
Professor Duk-Woo Park said, "We expect that the results of this study will resolve concerns about the risk of cerebral thromboembolism due to leaflet thrombosis after TAVR since we have found that there was no association between subclinical leaflet thrombosis and cerebral thromboembolic lesions.”
"Since leaflet thrombosis, confirmed on CT scans, is only an imaging phenomenon, it is desirable to select the type of antithrombotic therapy by comprehensively considering the clinical condition, stability, and effectiveness of each patient," he said.












