-
- Global AMC MENU
- NEWS
- HEALTH
- PEOPLE
- Introduction
Professor Wonjun Ji, Division of Pulmonology and Critical Care Medicine
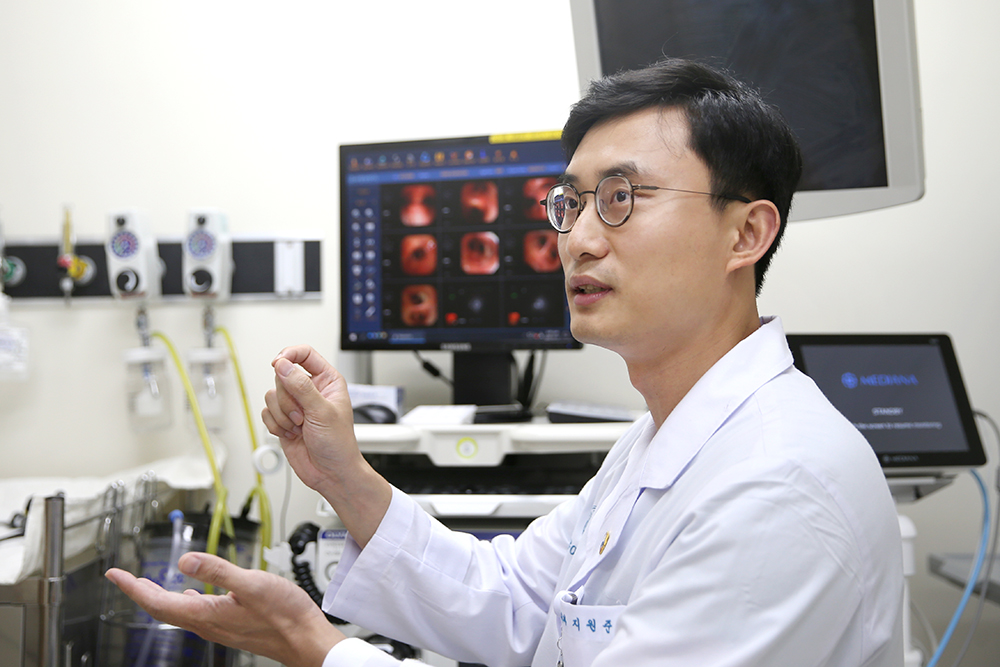
‘It will be helpful but risky…’ A patient arrived at the emergency room with airway obstructed by a tumor. If sputum or bleeding leads to sudden airway obstruction, it can result in death due to the inability to breathe. After carefully considering the challenging situation, Professor Wonjun Ji performed a rigid bronchoscopy. “Completing a procedure motivates me to take risks and give my best. Although rare, losing a patient during a procedure further reminds me of my responsibilities as a practitioner. I am gaining experience in selecting patients who will benefit the most from my procedures. Of course, the most significant lessons come from the patients themselves.”
Thorough Contemplation and Fast Execution
During high school, Professor Wonjun Ji dreamed of creating a new drug that would lead South Korea. This idea came after he fell in love with biology and genetics while preparing for a biology competition at the suggestion of his homeroom teacher. An encounter with clinical medicine in medical school doubled his enthusiasm. The process of investigating patients’ symptoms, identifying the beginning and progress of problems, and searching for solutions was like solving exciting mysteries. Starting from his third year in medical school, he spent summer vacations at the hospital as a sub-intern. During his internship, he was given a rare opportunity to serve as the attending physician for Ward 62, which boosted his confidence in working with patients. He also made an early decision to specialize in Pulmonology and Critical Care Medicine. “I think I was lucky. I tend to overthink, but I had the privilege of meeting great mentors who provided timely advice and suggestions as I needed them. That helped me make important decisions quickly, explore more actively, and gain enjoyment and confidence.”
Professor Wonjun Ji primarily specializes in lung cancer diagnosis and bronchoscopy intervention. Lung cancer is often detected at advanced stages, and even in the early stages, the 5-year survival rate is lower than for other cancers. Fortunately, an increasing number of measures are becoming available for patients because diagnostics and treatments in this field are advancing rapidly. When patients come to express their gratitude after a safe transition to subsequent treatment or gradual recovery, he is filled with joy, as if he has been running toward that moment all along.
Bearing the Weight of Life
A patient in his 60s was admitted to the hospital with suspected lung cancer. The Medical Emergency Team (MET) was called because he suddenly developed shortness of breath over the weekend. Half of his lungs were found to be non-functional due to a tumor blocking the airway. Since a respirator could not sustain him, a heart-lung machine, a life-saving device, had to be employed. Professor Wonjun Ji placed hope in the fact that the patient was relatively young and had healthy lungs except for the peri-bronchial tumor. After a thorough discussion with the patient’s family, they decided to proceed with a rigid bronchoscopy. The next day, the heart-lung machine and respirator were removed from the patient, who managed to climb the stairs to a regular ward in three days. “The patient and his family, once on the verge of a sudden separation, have been thanking me whenever they have an outpatient appointment for three years. I am delighted for them, of course. Even though I encourage them not to visit too frequently because they live quite a distance away, it is of no use (laughs).”
When he began performing rigid endoscopy in 2018, he experienced a great deal of stress. What was even more challenging than the tension and burden was the guilt he felt when unable to stop uncontrollable bleeding in a patient and had to declare the patient’s death. He could not help but wonder, ‘Could I have hastened the patient’s demise?’ However, the patient’s family appreciated his willingness to take risks. “I was told that patients with similar symptoms were transferred to other hospitals for treatment just a few years back when I was in my residency. Now, my focus is on being able to help them.”
There are principles to consider when deciding to perform a procedure. It should be determined that the procedure can help patients breathe comfortably and lead to subsequent treatments for life extension. Additionally, both the patient and their caregivers should fully comprehend and consent to the procedure’s risks and benefits. Professor Wonjun Ji exercises caution when contemplating a procedure, avoiding hasty decisions based solely on technical feasibility. “Approximately 40 cases are performed annually, with the number increasing each year. Given the high-risk nature of the procedure, I always closely consult with professors from various medical departments and seek mutual assistance to overcome critical moments.”
Closer to His Dream Through Trials and Challenges
Professor Wonjun Ji sees 60 to 80 new lung cancer patients every month. The standard approach to treating these patients involves percutaneous biopsy, achieved by inserting a needle into the lungs. However, in some cases, accessing the affected area can be challenging, or there may be a high risk of complications. To address these issues, Asan Medical Center is equipped with electromagnetic navigation bronchoscopy and radial endoscopic ultrasonography, utilizing all available endobronchial diagnostic techniques in South Korea for diagnosing peripheral lung lesions.
While bronchoscopy is currently primarily employed for diagnostic purposes in the peripheral lung areas, Professor Wonjun Ji is actively involved in a national project aimed at developing devices for therapeutic purposes. “Research emerging from a clinical setting fosters a different mindset and attitude. Engaging in various clinical studies allows me to indirectly contribute to new drug development or the introduction of innovative medical techniques, something I aspired to since high school. My ultimate dream and goal are to become a doctor who offers the highest level of diagnosis and treatment in the field of interventional bronchoscopy. I hope to witness more of my patients breathe freely.”












