-
- Global AMC MENU
- NEWS
- HEALTH
- PEOPLE
- Introduction
Advancing Patient-Centered Care and Safe Medical Services
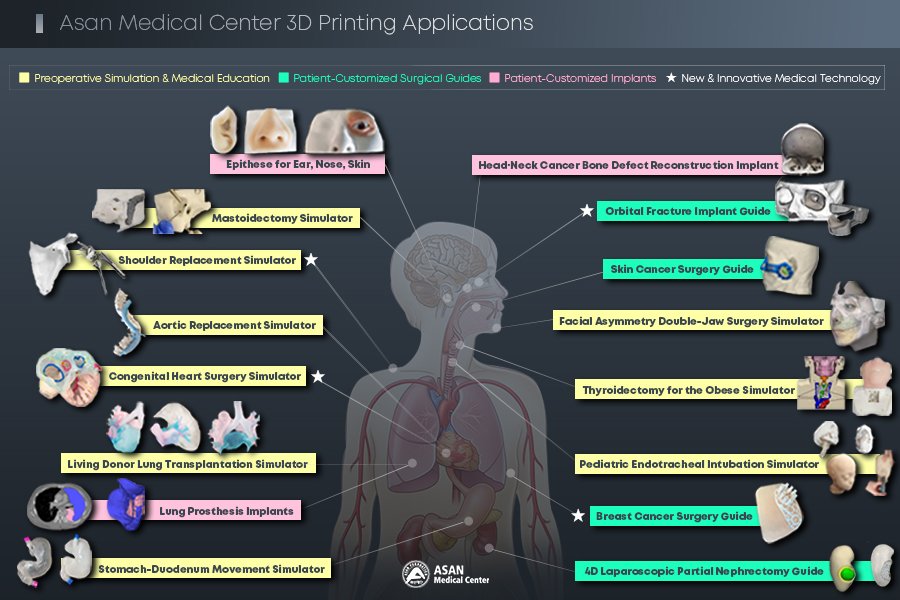
Over the past decade, Asan Medical Center has leveraged 3D printing technology to develop custom medical devices, aiding medical professionals in complex surgeries and promoting innovative treatment methods.
Medical Imaging & Intelligent Reality Lab (MI2RL), led by Professor Namkug Kim of the Department of Convergence Medicine, has collaborated with various departments since introducing 3D printers in 2014 for research purposes.
3D printing has been instrumental in creating patient-customized simulators, reducing trial and error in complex procedures and first-time surgeries. Operations for critically ill patients with intractable diseases require elaborate planning and execution, and it was 3D printing that enabled the simulation of such operations.
This technology has been crucial for preoperative planning and simulation for practice in advanced surgeries, such as Korea’s first living donor lung transplantation (Professor Seung-Il Park of the Department of Thoracic & Cardiovascular Surgery and his team) and pediatric congenital heart surgery (Professor Tae-Jin Yun of the Division of Pediatric Cardiac Surgery and his team).
A notable recent achievement is the application of 4D printing technology in partial nephrectomy for kidney cancer, where a customized surgical guide was developed. A research team led by Professor Yoon Soo Kyung of the Department of Health Medicine added a new dimension of ‘time’ to the traditional 3D-printed kidney cancer surgical guide. The guide, reduced in size, passes through a 1cm laparoscopic port to enter the body, reverts to its original shape, and shrinks again after a set time. The team created a 4D-printed surgical guide customized for kidney cancer using this property.
3D printing is beneficial in facial reconstruction (Professor Jong Woo Choi of the Department of Plastic Surgery and his team). Artificial bones are printed to replace defects caused by cancer or trauma immediately. The team led by Professor Jong Woo Choi also researched facial prostheses (epitheses), considering skin texture and color to allow ear or nose defects to look natural.
A lung prosthesis implant (A team led by Professor Yong-Hee Kim and Professor Jae Kwang Yun of the Department of Thoracic & Cardiovascular Surgery) that can minimize side effects caused by empty spaces from post-lung resection is being developed and undergoing animal testing.
A temporal bone mastoidectomy simulator (Professor Jong Woo Chung of the Department of Otolaryngology-Head and Neck Surgery and his team) prints out the anatomical structure of the ear, nose, and throat and enables medical professionals to practice drilling. A published study evaluated its educational utility, confirming its value in training environments.
A breast cancer surgical guide developed by Professor Beom Seok Ko of the Division of Breast Surgery and his team was designated as an innovative medical technology, and research on improving surgical accuracy using 3D modeling and augmented reality is underway.
These achievements have gained recognition by being designated as new and innovative medical technologies, by publications in journals, and by receiving academic awards.
Four projects, including a medical guide for artificial shoulder joint replacement (Professor Kyoung-Hwan Koh of the Department of Orthopedic Surgery and his team) and an orbital fracture implant production guide (Professor Ho-Seok Sa of the Department of Ophthalmology and his team), have been designated as new or innovative medical technologies.
The 4D kidney cancer guide and the idea of lung prosthesis implant production have won awards at the Radiological Society of North America (RSNA) 3D Printing Special Interest Group.
A study was published in the Journal of American College of Cardiology, ‘JACC: Cardiovascular Imaging,’ revealing that a pediatric cardiac surgery guide (Professor Tae-Jin Yun of the Division of Pediatric Cardiac Surgery and his team) incorporated into the treatment process of patients with congenital heart disease has changed treatment methods in 5 out of 14 patients.
The study on aortic artificial vessel replacement (Professor Joon Bum Kim of the Department of Thoracic & Cardiovascular Surgery and his team) gathered significant attention as it was published twice in the Journal of Thoracic and Cardiovascular Surgery of the American Association for Thoracic Surgery and received a two-page commentary.












